
An ACC review released to RNZ shows it is paying 40 percent more than rates across the Tasman. Photo: 123RF
This is the third in an RNZ series about the growing pressures, profits and waiting lists in the fraught field of radiology, and the jammed bottleneck that most patients must pass through.
New Zealanders are paying over the odds for radiology scans compared to Australia, the UK and some other countries.
An ACC review released for the first time to RNZ shows it is paying 40 percent more than rates across the Tasman.
In another seven-country chart, New Zealand ranks second only to the US for the price of the most popular scan, an MRI - $750 versus $1400, compared to just $190 in the Netherlands, as of 2017.
"The average New Zealand insurance price for an abdominal MRI is 66 percent above the UK price, and abdominal CT is 23 percent above," said the review, citing 2020 International Federation of Health Funds figures.
Read the full High Tech Imaging Review
ACC, the largest single funder of high-tech imaging (HTI), has responded by freezing the rates it pays private providers.
It is also now investigating ways it might change the scanning funding model.
This comes amid runaway demand - 130,000 scans worth $112m last year, representing a $9m budget blowout. Cost and volume growth was running between 7 and 17 percent, the review said.
It also said private providers were charging private patients 17 to 53 percent more than the ACC rates.
ACC ordered the review to help "improve the financial sustainability of the service".
'Confusing and stressful'
"HTIs are no longer the exception and are fast becoming the norm," it said.
"Volumes and demand will continue to grow" despite a system that "can be both confusing and stressful for all sector participants".
The review recommendations could pave the way for yet more scanning: One recommendation is that, when in doubt, ACC should make it mandatory for doctors to order a scan.
"The growth in HTI use suggests that this is happening already," ACC told RNZ.
"We recently expanded a pilot that allows GPs to refer their patients for an MRI. This service is now available to GPs anywhere in New Zealand."
It might expand this to include other health professionals, ACC said.
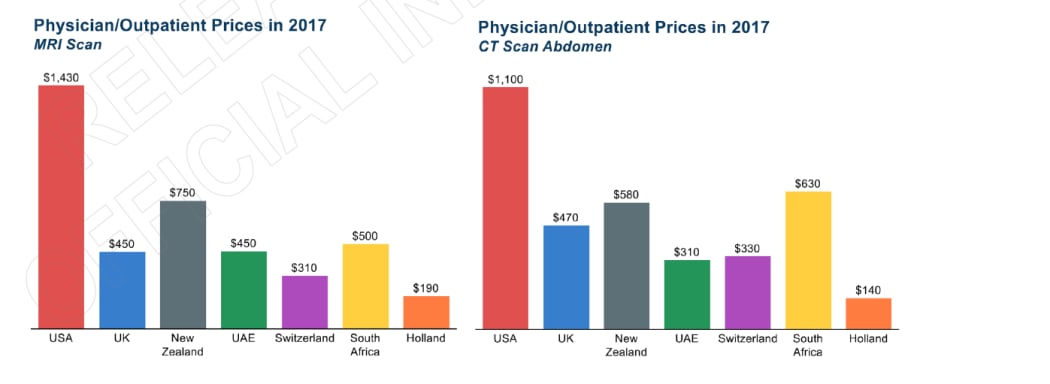
A comparison of prices for scans between countries based on 2017 statistics. Photo: Supplied / ACC
The price comparisons showed that in 2021 Australia's Medicare scheme was paying out 44 percent less for an MRI and 39 percent less for a CT scan than ACC (even allowing for the fact Medicare does not always pay the full scan cost).
At least two local public hospitals had outsourcing rates $100-$150 under the ACC rates, it said (outsourcing is where they pay private providers to do scans to cut public queues).
Scans are paid for by ACC for trauma injuries, from public hospital budgets, from outsourcing, by insurance and by patients themselves.
ACC's 2022 fee schedule is $799-$1089 for a whole raft of different MRI scans, and $450-$950 for a range of CTs.
In 2016, it covered just 10 special types of scan worth just hundreds of dollars each; by last year that had expanded to 18 special scans, some costing $1000-$4000 each.
The high rates were not due to too few machines: OECD figures show New Zealand in the middle or higher end of the pack for CT and MRI machines per capita.
"This rules out the size of the market being a driver of cost," the external reviewers told ACC.
The agency detailed the unflattering comparisons in a memo to tell providers why it was not raising what it paid them this year.
"The sector is sustainable," it said, adding this was demonstrated by six new practices being set up by private providers.
It asked for feedback on its freeze decision but has heard back from just one radiology company so far, ACC told RNZ.
"We have also offered to review our HTI suppliers' actual costs to ensure we're paying sustainable rates."
'Where are they getting the data from?'
The ACC reviewers noted with surprise they were "unable to find a national inventory of MRI machinery" so they created one.
A health economist questioned how ACC settled on what to pay private providers, given there are such big gaps in data about radiology.
"How did those figures come about in the first place?" asked Professor of Health Economics Paula Lorgelly.
"Where are they getting the data from that informs those reimbursement levels?"
She went looking for the data ACC may have used, but could not find it.
The contrast was with Pharmac, which had a strong evidence base when it negotiated deals to get drugs.
"There seems to be a dearth of evidence on radiology and radiologists, little by way of updated facts," Lorgelly said.
Public costs were not the same as for private practices, but were vital if the health reforms were to be efficient and fair, she added.
"We need to understand who's delivering care and who's getting care.
"On the delivery side, it looks like there is not just enough information to understand who's in the workforce, who works privately, who works publicly, therefore, what is the capacity of the workforce to increase the number of images and scans that it does?"
An audit of scanning equipment and its age was important, and where it was, she said.
"This is probably one of the messier parts of the healthcare system because of the mix of public and private providers.
"But it's also our key to really understanding it, because there's a huge amount of venture capital that can come into the space of radiology, setting up new clinics, and taking away potentially public workers into that private space."
ACC said its next step was to get another external review done of HTI procedures, before it decided on any changes.
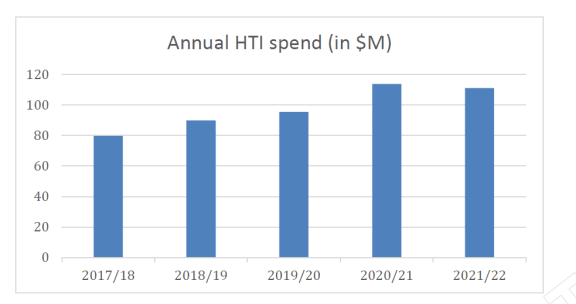
High-tech imaging spending, as supplied by ACC. Photo: Supplied / ACC
Its funding model was last changed 13 years ago, in 2009, when it cut rates by a fifth.
Since then inflation had pushed them back up.
Lorgelly questioned if any ACC funding redress might mean a withdrawal of services.
"Will it mean these mostly private clinics have to generate demand?"
Just under a third of ACC's total payouts last year went to Pacific Radiology, that dominates south of Auckland. Pacific is now part of a group majority-owned by investment company Infratil.
The average spend per ACC claim in 2020 was $933. MRI makes up 80 percent of demand.
"Techniques have improved so much over time that physicians may be using them for concerns that might not have prompted imaging in the past," its review said.
CTs were now the go-to for detecting pulmonary embolism "and this has undoubtedly contributed to the dramatic rise in costs associated with imaging of the chest".
The review looked at how population growth and movement might change demand.
"Too few units may lead to access problems in terms of geographic proximity or waiting times.
"If there are too many, this may result in overuse of these costly diagnostic procedures, with little if any benefits for patients."
International research has shown that the availability of extra scanners can actually generate unnecessary scanning.
A Health Economics journal article in 2020 said of "supplier-induced" demand "that financial incentives and production processes may override clinical guidelines and the patient's best interest".
"In particular, the possibility to self-refer patients generates strong incentives to induce demand ... even for procedures with health risks."
Unnecessary CT examinations could cost a lot and expose patients to "high doses of medical radiations".
Lorgelly said scanning was "very sensitive to financial incentives and this is heightened when non-radiologist physicians own imaging equipment and self-refer patients".




