
In a report done earlier this month, radiologists have detailed problems with the radiology information systems the hospitals use. File photo Photo: Gorodenkoff Productions OU / 123RF
Health authorities have been given a behind-closed-doors warning poor radiology reporting throughout the central region is endangering people's lives.
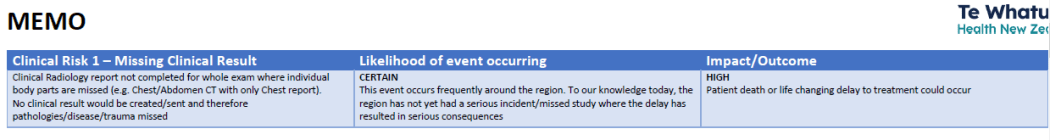
A new internal report to Health NZ, obtained by RNZ, lists five frequent failings that are a threat to treatment, including of serious conditions like cancer.
It says not once but four times:
"Likelihood of event occurring - Certain. This event occurs frequently around the region.
"Impact/Outcome - High - Patient death or life changing delay to treatment could occur."
In the report done earlier this month, radiologists describe how dysfunctional IT systems are losing information, failing to link vital reports together or logjammed, and how some staff are so "jaded" that they are now resisting "upgrades" because these have never worked before.
The problem is with the radiology information systems (RIS) the hospitals use. These are often failing to link all of a patient's scans together - which can make all the difference between a low risk or a high risk diagnosis, the doctors reported.
The "alarming" risks have persisted for years in the central region of Wellington, Hawke's Bay and Manawatū, covering a million people, the report said.
Most other regions use a different type of RIS.
The radiologists told Health NZ that as far as they know, mistakes had always been caught and not caused a "serious incident" yet - but that Te Whatu Ora must address them.
For all four top risks, all fix-it attempts so far had been "ineffective".
"We currently do not have a clinically safe resolution," the report said.
It is an example of the public health system's legacy technology now playing up; official reports have said will cost $2 billion-plus to fix nationwide.
RNZ has been told the hospitals in some cases have not helped themselves.
"The main issue is the DHB (mainly Capital and Coast) has not got their IT infrastructure in line and have not for years," a source said.
A new internal report to Health NZ, obtained by RNZ, lists five frequent failings that are a threat to treatment. Photo: Supplied
'They are not interested in potential improvements'
Technicians take the scans and use RIS to send them in an electronic package to a radiologist.
This doctor relies on getting a full set of scans in order to produce a single, crucial report on what is wrong.
The report said each of the following events "occurs frequently around the region" and each is life-threatening:
- Missing clinical results - multiple scans are taken of a patient's different body areas - but not all of them come up in RIS. "No clinical result would be created/sent and therefore pathologies/disease/trauma missed." An example was given of a doctor just happening to notice a chest scan that did not upload alongside an abdomen scan; a lung nodule on its own only warrants being put on the six-month check-up list - but matched with a tumour in the abdomen the cancer threat "significantly changes".
- Delayed or missed communication of clinical results - Reports are not getting through reliably and accurately to the referring clinician and GP, generating "confusion" and possibly "delayed/missed treatment decisions". Hawke's Bay and MidCentral are manually printing out each patient's report, twice, at a cost of perhaps "hundreds of thousands of dollars" a year. Wellington Hospital is now manually searching through other districts' reports on "each individual patient" to make sure everyone gets them.
- Outsourcing is jammed - Public hospitals are relying on private providers to read and report on scans, especially after-hours and at weekends, but are too slow and uncoordinated to secure deals - or drive prices down: "We currently negotiate and have separate agreements across all districts with the same private providers."
A fourth life-threatening risk that is listed as not being reported back on, but as nevertheless "certain", is that:
- End users are not speaking up - "Districts that have been on the [regional] RIS for a long period are extremely jaded and do not raise clinical risks that they feel have been made clear multiple times." The report said just a two-week period earlier this month, Hawke's Bay radiologists refused to raise loading issues. "They have dealt with extremely long and unacceptable loading times for years now without resolution."
In Hawke's Bay, and at MidCentral, clinical and operational leaders had balked at a potential upgrade to a system (PACS) that is a subset of RIS: "They are not interested in potential improvements as from their perspective, they have only had bad experiences in 'upgrades' or changes."
A fifth problem, of the RIS going slow or stopping, is adding to long public waiting lists. This contributes to scanning machines being left idle, compounded when there are not enough radiologists to report the results.
The IT issues were making it much harder in Wellington to use private providers to do reports after-hours and at weekends, which could hugely help, sources said.
Only one "somewhat effective" mitigation is listed, to try to increase capacity; however, the remedy, "do more in less time to catch-up", could not be sustained, the report warned.
The public system is faltering even as the private health-tech sector is burgeoning, generating an estimated $2.85b in 2020.
Risks 'mitigated by the tireless work of our clinical staff' - Te Whatu Ora
Te Whatu Ora declined to be interviewed but in a statement said an "intensive effort" is underway to resolve the "flaws".
"While some of the issues identified have proven difficult to resolve, any risk to patients has been mitigated by the tireless work of our clinical staff who manually check work lists and distribution of patient reports," said central region's radiology clinical network director Jaco van der Walt.
"We are not aware of any adverse patient outcomes that may have resulted from the issues identified with the regional RIS."
Health NZ interim regional director Russell Simpson said the problems largely came to light during a recent rollout in Wellington of shared regional RIS systems.
This flies in the face of the radiologists' report stating: "These risks have been present for a long time in many districts."
Simpson echoed the report when he noted some recent gains made in system performance - though the report went on to say the approach to secure the gains "is not effective" in an environment of intense pressure.
The regional rollout to increase shared information had been put on hold at Hutt and Wairarapa hospitals until the problems are fixed, Simpson said.
International Accreditation New Zealand (IANZ) accredits hospitals and can suspend them if services are not up to scratch.
Chief executive Brian Young said he was aware of the clinical risks posed by RIS in the region.
"The review of a provider's RIS is a core component of all of our radiology assessments," Young said.
"IANZ understands and respects the need for timely provision of diagnostic imaging for all patients, and in the interests of safe patient care works cooperatively with all providers to ensure effective management of potential non-compliances before they reach the threshold of suspension.
"It goes without saying that the ultimate desired outcome for all involved, including IANZ, is the safe and accurate delivery of results and the best possible outcome for the patients."
The region's RIS is largely supplied by Philips Health Systems, some of it legacy technology developed by Carestream, which sold its global health info systems to the Dutch multinational in 2019.
In a statement, a Philips spokesperson said they had been working closely with Te Whatu Ora and clinical teams to address issues.
"We're glad that systems upgrades and improvements are being prioritized and see this as a positive step towards mitigating these issues in the future.
"Patient safety and wellbeing is at the heart of everything we do at Philips. We will continue to support our customers and clinicians to ensure critical radiology services are meeting patient needs."




